Thank you for the kindness and care shown to me and my husband during our cataract operations. You gave us confidence and we are both recovering well
By Mr Ramy Bassily | August 1st, 2017
Keratoconus
What is Keratoconus?
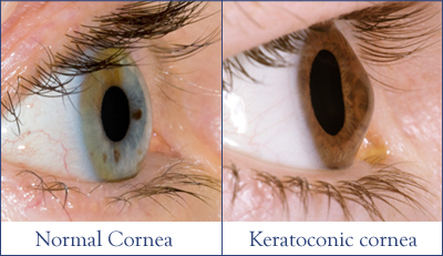
Keratoconus is a disease of the cornea; this is the transparent window at the front of the eye that makes it possible to see your coloured iris and central round black pupil when you look in the mirror. To maintain clear vision the cornea must maintain a spherical shape. Keratoconus is the progressive thinning of the cornea that results in a bulging (cone-like) shape. This makes it more and more difficult to maintain a clear focus with your vision.
Who gets Keratoconus?
The exact reason for this disease process is not fully understood but we do know that approximately 1 in 1000 people have this condition but this rate is higher in Asian ethnicity. Although there are genetic factors it does not tend to be passed down from family members. It is known to be associated with other conditions, particularly asthma and eczema. It is also more common in patients with Down’s syndrome and Marfan’s as well as other skin and joint conditions.
How does this condition affect me?
Initially you may not notice any visual problems. However, as the condition progresses you will find the vision becomes more blurred. Glasses will help improve the vision in the milder stages but further deterioration will lead to symptoms of light sensitivity and inadequate vision with glasses requiring specialized contact lenses. The majority of people do not progress worse than this, but in the most advanced stages of the disease the bulging of the cornea can lead to episodes of pain and eventual scarring of the cornea.
Although this condition is bilateral it is often asymmetrical and it is not uncommon for one eye to be hardly affected at all.
The rate of progression is highly variable from patient to patient, it is not fully understood why some people can progress minimally while others can have advanced disease.
However, the tendency is for the condition to slow down in progression once 30 years old and almost always has completely stopped progressing by the age of 40.
What can I expect from my visits to the hospital?
In the eye clinic you will have various tests including a vision check and a thorough eye exam. You will also have the shape of the cornea measured on a special machine; this is called topography and is the gold standard in diagnosing and monitoring keratoconus, it will also measure the thickness of the cornea.
Usually on a separate visit you may attend our specialized contact lens clinic for a personalized assessment and contact lens fitting.
On you visit to the hospital where possible please can you:
- Bring copies of any prescriptions for glasses or contact lenses from your optician
- Remove your contact lenses three days prior to your visit as this will alter the shape of your eyes
What treatment is available to improve the sight?
In the first instance, it is usually possible to maintain very good vision with glasses. The next stage is to attend the contact lens clinic, our specialized contact lens practitioners can often fit lenses with excellent vision even in advanced disease.
When contact lenses are no longer adequate we will discuss with you the surgical options. Treatments vary and your doctor can explain the options available. The mainstay of surgical treatment is a corneal transplant.
Be reassured that only one patient in every twenty with keratoconus goes on to require a corneal transplant. The number of patients requiring transplants is becoming even less since the advent of treatments to halt the progression of the disease. More information on corneal transplant surgery can be provided when needed.
What treatment is available to stop the keratoconus progressing?
It is very likely that the condition can deteriorate more rapidly in patients who rub their eyes. This tends to be a problem for patients with allergies and eczema. As such we recommend that you remember as best as possible to not rub the eyes.
A specialized procedure called Collagen Cross Linking (CXL) has been shown to stop or significantly reduce the progression in nine out of ten cases. This procedure has also been approved by NICE (National Institute for Clinical Excellence) to treat progression in keratoconus.
CXL is a minimally invasive procedure that lasts up to 30 minutes. It involves placing vitamin B2 (riboflavin) on the cornea while shining ultraviolet light onto the eye. By doing so fibres in the cornea are encouraged to bond or cross-link to hold the shape of the eye more rigidly. This treatment accelerates the natural age-related stiffening of the cornea.
If you are suitable for this treatment your doctor will explain your options for treatment, the risks involved and what to expect.